Vesicular Skin Lesions: Causes, Symptoms, Diagnosis, Treatment
From allergies to lifting weights without gloves, anything can cause this type of skin blisters.

Image: Shutterstock
Vesicular skin lesions are tiny, liquid-filled, blister-like bumps on your skin. The fluid inside that sac can be clear or mixed with pus or blood. Multiple reasons may cause blisters on your skin. This may include friction or infection. However, in some cases, vesicular lesions may indicate serious underlying conditions. Read this article to understand the causes of vesicular skin lesions and learn about the diagnosis, treatment, and prevention tips.
In This Article
What Is Vesicular Skin?
Vesicular skin lesions are nothing but blisters. They are small sacs filled with either clear or pus-colored fluid. They are typically 5-10mm in diameter. They are delicate and can burst due to pressure or friction. When a vesicle bursts, it becomes a vesicular eruption. Once they burst, the liquid spreads to the surrounding skin and leaves a white or yellow flaky crust when it dries. If the diameter of the lesion is more than ½ cm, it is called bullae.
In the next section, let us understand some of its symptoms.
Symptoms Of Vesicular Skin
Vesicular skin lesions can be easily identified. They develop on the surface of your skin and appear to be swollen and filled with liquid. They can cause redness, itching and can be painful to touch. Over time, they generally disappear by themselves. It is important to note that hives and vesicular skin lesions are different skin conditions. Hives are itchy and raised and can cause swelling, while vascular skin lesions are fluid-filled blisters.
While the symptoms of vesicular skin lesions may be easy to detect, the causes are numerous. In the upcoming section, let us look at some of the causes of vesicular skin lesions.
What Are The Causes For Vesicular Skin?
Vesicular skin lesions or blisters can be caused by something as benign as lifting heavy weights at the gym without gloves, breaking into a new pair of shoes, or suffering a burn on your skin. Some of the more serious causes are as follows.
- Frostbite
If you’ve got frostbite, bullae (vesicular skin lesions) will begin to appear when the affected area is re-warmed (1).
- Allergic Contact Dermatitis
It is common for vesicular skin lesions to appear in acute cases of allergic contact dermatitis. It is a type of skin inflammation caused by the aggravation of contact dermatitis due to allergen or irritants (2).
- Covid -19
Recent studies have suggested that vesicular skin lesions may be one of the side effects of Covid-19 (3). A study analyzed 24 patients who showed symptoms of Covid -19. Out of the 24, 19 of them developed vesicular skin lesions after the onset of Covid-19’s symptoms.
- Bacterial And Fungal Infections
Bacterial and fungal infections can also cause vesicular skin lesions to manifest. Cuts and wounds on your skin not cared for may cause you to come in contact with these bacteria and fungi. Erysipelasi A disease characterized by large, red bumpy patches on the skin caused by a bacterial infection. , Herpes zoster, and Herpes simplex are some of the most common infections to cause vesicular skin lesions (4).
- Chickenpox
Chickenpox is characterized by itchy vesicular skin lesions. These lesions appear in crops and progress from red spots to blisters filled with clear fluid (5). After a few days, they turn to pustules, which rupture and crust over. The number and distribution of these lesions can vary, and they make the condition highly contagious.
- Impetigo
Impetigo, another highly contagious bacterial skin infection, also causes vesicular skin lesions. These lesions typically start as small blisters or pustules that may burst and ooze fluid. They eventually form honey-colored crusts, and can be itchy and painful (6). Impetigo often appears around the face, hands, and extremities.
It is important to seek medical assistance in the above cases of vesicular skin lesions. Let us understand what other situations will require medical assistance.
When To See A Doctor?
It is possible to treat most vesicular skin lesions and blisters with the help of OTC medications. If you start to feel pain, dizziness or are having an allergic reaction to OTC medications, seek medical assistance immediately.
In the next section let us understand how vesicular skin lesions are diagnosed.
How To Diagnose Vesicular Skin Lesions?
If you notice strange vesicles that appear on your skin, you should consult with your doctor. You will be asked questions about your recent medical history or any medications that you may be taking. This is to help determine if any pre-existing medical condition is related to your vesicular skin lesions.
The doctor will also examine your skin to diagnose the cause. If your doctor is unsure of the diagnosis, they may ask you to undergo a few tests. The doctor may collect a sample of the fluid and perform a biopsy of the skin tissue of the vesicle. This is sent to a laboratory for analysis that will help arrive at a final diagnosis.
Once your diagnosis is complete, you will know if the vesicular skin lesion is benign or is it an underlying medical condition that is causing these lesions.
 Quick Tip
Quick TipIn the next section let’s find out how vesicular skin lesions are treated.
Treatment Options Available For Vesicular Skin
Treatment for vesicular skin lesions varies from case to case. It is strongly recommended that you do not pick or scratch open the vesicle. If it becomes too painful and swollen, you can go to a doctor, and they will safely drain the fluid. This allows the skin to heal effectively and avoid the risk of developing an infection.
In most cases, over-the-counter medications(OTC) are prescribed by your doctor as part of your treatment. For cases where vesicular skin lesions are caused due to allergic reactions, or poison ivy, antihistamines ointments are prescribed.
In the case of vesicular skin lesions caused by Covid-19, antihistamines, anticoagulants, and corticosteroids are prescribed as part of the treatment (7). Lesions caused by burns will be treated with burns creams and oral antibiotics.
Avoid self-medication and consult a doctor in these cases.
 Trivia
TriviaIs there a way to prevent vesicular skin lesions? Let us find out in the next section.
How To Prevent Vesicular Skin?
Vesicular skin lesions are not always preventable. Especially genetic lesions like Epidermolysis bullosa simplexi A genetic condition caused due to skin fragility that makes the skin develop blisters and erosions upon even mild friction. . This is a genetic condition that causes your skin to be fragile and makes it prone to blistering (8). Allergic vesicular lesions also can’t be prevented. You have to take necessary precautions to avoid allergens that trigger this condition. You should also maintain good skin hygiene and use antibacterial soaps to wash your skin to protect it from infections.
Infographic: 4 Major Causes Of Vesicular Skin Lesions + Treatment Options
Vesicular skin lesions or blisters are liquid-filled bumps that appear on the skin. They can be painful and cause discomfort. Keeping them untreated may lead to further infection. The infographic below highlights the 4 major causes of vesicular skin lesions and the best ways to treat them. Check it out to learn more.
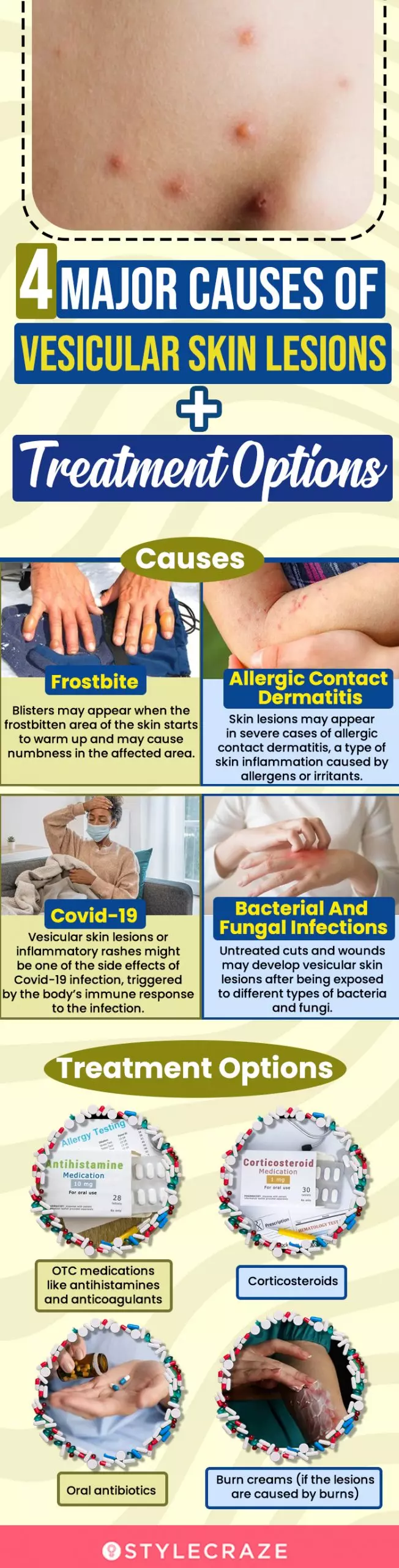
Illustration: StyleCraze Design Team
Vesicular skin lesions are small bumps filled with blood or pus accompanied by redness, itchiness, and pain. Factors such as genetics, infections, frostbite, or heavy lifting may lead to the development of painful vesicular skin lesions. If your vascular skin lesions are painful and swollen, consult your doctor. They may prescribe OTC creams, ointments, or medications to treat the condition. While vesicular skin lesions cannot be completely avoided, taking preventive measures such as maintaining excellent personal hygiene can reduce your chances of developing vesicular skin lesions.
Frequently Asked Questions
Can eczema cause vesicles?
Yes, eczema can cause vesicles. The pus-filled itchy blisters usually form on the hands, sides of the fingers, or on the soles of the feet. These require prompt medical attention to avoid the formation of deep fissuresi A painful condition where the skin at the bottom of the heels dries out, hardens, and is calloused, resulting in bleeding. from scaling skin and to prevent the condition from becoming chronic.
Is shingles a vesicular rash?
Yes, shingles present vesicular rash as one of the primary symptoms. The condition, caused by the Herpes zoster virus, leads to the formation of itchy vesicles on the skin that typically appear within 3-5 days of contracting the infection.
Is there a risk of vesicular skin lesions recurring after successful treatment?
Yes, vesicular skin lesions may recur if the initial cause is avoided such as re-exposure to allergens in the case of vesicles caused by atopic contact dermatitis.
Is Vaseline good for vesicular lesions?
Vaseline may help keep the affected area moisturized and aid the healing process. However, there is no scientific proof that it may help treat vesicular lesions.
Is Neosporin good for vesicular lesions?
It may help prevent further chances of bacterial infection in the existing vesicular lesions. However, it is also known to cause skin irritation in sensitive skin. Hence, it is advisable to consult your doctor before using Neosporin on vesicular lesions.
Key Takeaways
- Vesicular skin lesions are small, liquid-filled blister-like bumps on the skin measuring 5-10mm in diameter.
- They can cause irritations, redness, and discomfort when touched.
- Breaking in new shoes, getting a burn on your skin, frostbite, or allergic contact dermatitis, can induce vesicular skin lesions or blisters.
- In most circumstances, you may be able to treat them using over-the-counter drugs. However, if that does not work, you must contact your doctor immediately.

Image: Stable Diffusion/StyleCraze Design Team
Learn about the different types of vesiculobullous lesions, including bullous pemphigoid, pemphigus vulgaris, and dermatitis herpetiformis. Understand their classification and how to diagnose them from the insightful video below. Check it out now!
References
Articles on StyleCraze are backed by verified information from peer-reviewed and academic research papers, reputed organizations, research institutions, and medical associations to ensure accuracy and relevance. Read our editorial policy to learn more.
- Frostbite
https://www.ncbi.nlm.nih.gov/books/NBK536914/ - Contact Dermatitis
https://www.ncbi.nlm.nih.gov/books/NBK459230/ - Clinical and Histological Characterization of Vesicular Covid-19 Rashes: A Prospective Study in a Tertiary Care Hospital
https://pubmed.ncbi.nlm.nih.gov/32384180/ - Infectious Dermatoses That Can Manifest As Vesicles
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC6781845/ - Varicella-Zoster Virus (Chickenpox)
https://www.ncbi.nlm.nih.gov/books/NBK448191/ - Impetigo
https://www.ncbi.nlm.nih.gov/books/NBK430974/ - Identification Mechanism and Treatment of Skin Lesions in COVID-19: A Review
https://www.mdpi.com/1999-4915/13/10/1916 - Epidermolysis Bullosa Simplex
https://www.ncbi.nlm.nih.gov/books/NBK1369/ - Dermatology For the Practicing Allergist: Tinea Pedis and Its Complications
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC419368/
Read full bio of Dr. Tim Pearce
Read full bio of Anjali Sayee
Read full bio of Monomita Chakraborty






























